25.11.16
Social care could ‘undermine GM transformation and jeopardise NHS savings’
Significant issues with social care in Greater Manchester (GM) could ultimately destabilise the region’s transformational efforts over the next 18 months and put NHS savings at risk over the next four years.
In board papers published ahead of a GM Health and Social Care (GMHSC) Partnership meeting today, Steve Wilson, the organisation’s executive lead for finance and investment, pointed to two major issues with social care: the profiling of its financial gap, and the “mechanism by which the [2% precept] and the Better Care Fund will impact”.
GM has been allocated a sustainability transformation fund (STF) of £170m in 2020-21, which would potentially generate an NHS surplus by the end of the decade. However, given the level of risks and uncertainty in assumptions, the funding must be considered a contingency.
A major part of these uncertainties are the leftover questions around social care, which the organisation’s chief officer, Jon Rouse, recently underlined in an exclusive interview with PSE.
“These factors could undermine GM transformational efforts over the next 18 months and potentially jeopardise the achievement of NHS savings over the four years,” Wilson wrote in the paper.
The social care financial gap in GM stands at £176m at present. While the GMHSC Partnership has set out solutions to tackle the NHS deficit over the next four years, it cannot factor in the social care gap in overall deficit calculations “due to limited information being available to identify solutions to financial pressures within social care”.
Across the NHS, the current deficit – including commissioners and providers – stands at £897m, with a view to bring this to just £14m if planned solutions are implemented, according to GM’s STP submission. Factoring in social care, the overall deficit is expected to come down to £190m, compared to the current £1bn.
Amongst these planned solutions to bridge the money gap are efficiencies across commissioners (£134), providers (£418m), and specialised commissioning (£97), as well as better care (£233m) and the STF (£170m). These solutions were derived directly from the region’s 10 locality plans.
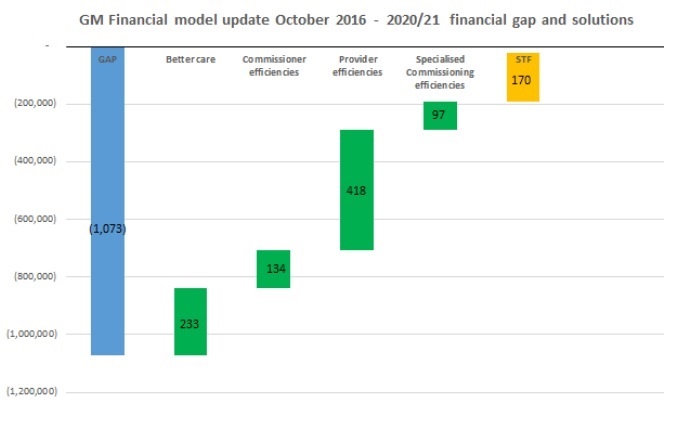 Click on the image to expand it in a new window.
Click on the image to expand it in a new window.
In the original diagram, there were a number of solutions to close the gap which were described as ‘transformational themes’, Wilson revealed – such as acute reconfiguration and pan-GM provider efficiencies.
“These themes remain the key building blocks of financial and clinical sustainability within GM; however these have now been subsumed within provider savings along with the ‘business as usual’ efficiencies,” he wrote.
Amongst the board papers was also GM’s six-month update report, which Rouse had told PSE's sister title NHE was expected to come out by the end of November. It explains how the region is faring across its four main pillars.